SAPHENOUS
 This is an often overlooked nerve block for ankle and foot procedures. This furthest extension of the femoral nerve has no motor component. It serves sensory innervation to the medial aspect of the calf including the ankle and some degree of the medial aspect of the forefoot. It also has a small contribution to the ankle joint. It is seen by some as an ‘add-on’ to a popliteal sciatic nerve block because it serves such a small area (and all superficial) that it may not seem worth doing. Maybe because of the failure rate associated with performing this block below the knee contributes to this view as well. Once the fibers reach the knee, they spread out in a wide fan-like distribution, and often some portion of it will likely evade our attempt at blockade (leading to a ‘partial’ failure anyway). Even when we block it here completely, local anesthetic is taken up at a higher rate (than if it were placed within a fascial plane), so the duration of analgesia is limited. Without ultrasound, we are left to perform this block blindly as a subcutaneous ‘half-ring’ block at the upper aspect of the medial calf, I have found this block is simple and quick (even with a catheter) when ultrasound is utilized, and it an integral component to foot and ankle procedures.
This is an often overlooked nerve block for ankle and foot procedures. This furthest extension of the femoral nerve has no motor component. It serves sensory innervation to the medial aspect of the calf including the ankle and some degree of the medial aspect of the forefoot. It also has a small contribution to the ankle joint. It is seen by some as an ‘add-on’ to a popliteal sciatic nerve block because it serves such a small area (and all superficial) that it may not seem worth doing. Maybe because of the failure rate associated with performing this block below the knee contributes to this view as well. Once the fibers reach the knee, they spread out in a wide fan-like distribution, and often some portion of it will likely evade our attempt at blockade (leading to a ‘partial’ failure anyway). Even when we block it here completely, local anesthetic is taken up at a higher rate (than if it were placed within a fascial plane), so the duration of analgesia is limited. Without ultrasound, we are left to perform this block blindly as a subcutaneous ‘half-ring’ block at the upper aspect of the medial calf, I have found this block is simple and quick (even with a catheter) when ultrasound is utilized, and it an integral component to foot and ankle procedures.
When I was first learning how to do continuous blocks, I didn’t know how to do a continuous saphenous nerve block. I had to do a continuous femoral block to cover the saphenous nerve (in conjunction with a continuous popliteal block) for an inpatient that had a huge nail put through his calcaneus into his tibia. Though it was worth losing quadriceps strength to get the necessary analgesia, it made ambulation quite an ordeal. Despite being so limited, the patient was still extremely grateful because he had the same procedure on the other leg previously and knew what he was missing (in terms of pain and opioid side-effects). Before the subsartorial technique was really talked about much and I was still new to ultrasound, I used a ‘soaker catheter’ below the knee a few times with success.
Today, I perform the subsartorial approach about a full hand breadth above the knee with the patient lying supine and the leg externally rotated. The sartorius extends from a lateral to medial direction and cuts across the vastus medialis (VM) distally. The VM is identified as the tear-shaped muscle medial to the knee. Even with obese patients, I try to feel for it or at least imagine its position with the sartorius running medial and posterior to it. I generally place the probe over the VM in a transverse orientation and direct it medially.
As the archetypal view below demonstrates, the muscle belly of the VM is seen completely covering the femur beneath. As you move medially, you are looking for the next ovoid structure that you encounter. That will be the Sartorius Muscle. Beneath it should be a pulsing artery, though it may not be directly under the center of the muscle. The artery will reside within a plane in or below the Adductor Canal. The muscles that you see would deep to the Sartorius are the Adductors. The left of the picture is medial.

In the following cadaver pictures, you can identify the sartorius muscle can be seen sweeping medially from the left of the image to the right to attach at the medial aspect of the knee. The vastus medialis is seen superior to the saphenous muscle. The saphenous nerve is deep to the saphenous muscle, and as it travels distally, it begins to migrate to the anterior aspect of the muscle. The sartorius muscle is pulled away in the next image to expose the saphenous nerve which is identified by the hemostats.
The Saphenous Nerve is not easily visualized underneath the sartorius muscle, but the Femoral Artery or the Descending Geniculate Artery (if you find it this distally) should be identified. Sliding the probe proximally and distally, you will see the Femoral artery diving deep to become the Popliteal Artery, leaving behind a smaller Descending Geniculate Artery. The roof of the Adductor Canal can be seen at times as a thickened fascial plane. Fortunately, you do not need to identify the nerve; just get your needle adjacent to the artery and inject. The nerve will become apparent at this point.
It is easier ergonomically to enter with the needle [nonmember]…
REGISTER for FREE to become a SUBSCRIBER or LOGIN HERE to see the full article!
[/nonmember]
[wlm_ismember]
between the VM and the Sartorius Muscle. It would also be helpful to stand on the same side as the leg you are blocking, but because of the way I tend to do the popliteal block (which I do first because it sets up slower), I am always on the opposite side of the leg I am blocking.
Aim at a point adjacent to the artery, not at the artery because a minor slip could cause you to have a big hematoma which looks bad and may interfere with block success). Initially, this is one reason I always travelled distal enough to encounter the Descending Geniculate Artery and went as far distally as possible. That way, if I hit it, it would be a smaller artery that was leaking, and it would be easier to stop the bleeding. I’ve seen this happen once; it was ugly, but their block still worked. The farther distally you go, however, the less distinct the structures become because they are smaller. Beyond that, you don’t want to take all day doing this because you do have two blocks to perform (If you are doing this one, you will certainly be doing a sciatic block, too). Now, I just go to where I see the structures and trace distally (if at all) to where I see them well enough and inject. Again, about hand breadth above the knee keeps me from looking around too much. I would go proximally if I were having any trouble.
The other reason to consider injecting distally is the theoretical concern that the higher you are, the more the local tracks proximally, and the risk of quadriceps weakness may be greater. I’ve never run into this problem, and I have examined (for inpatients) and questioned (for outpatients) thoroughly looking for it. A recent article in Regional Anesthesia & Pain Medicine by Saranteas et al (July-Aug 2011) addressed this as well and indicated that none of their 23 volunteers experienced a motor block. Another mitigating factor regarding potential motor block is the fact that most procedures for which this block is performed, the surgeon does not want the patient to be weight-bearing at all. The final word on this in my opinion is to have a very strong patient education infrastructure in place.
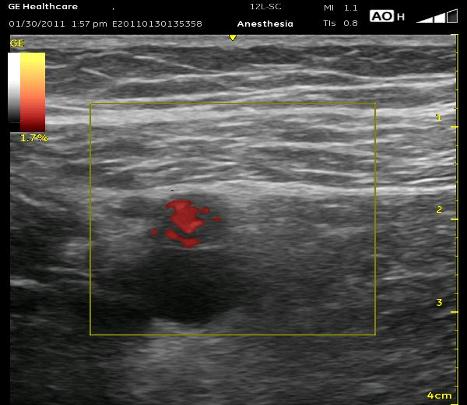
Here are a few technical points for this block. As I have mentioned in another section, take a moment first to pause then ‘bounce’ up and down to identify the Femoral Vein (adjucent to or below the Femoral Artery) or other vascular structures that may be collapsed. Color-flow may be helpful as well, especially the more distally you are. Note that in the ultrasound picture below, the subcutaneous tissue (when there is a lot of it) above the muscle can be mistaken for the muscle itself, and you will be looking too superficial for the artery. Try to notice the slight difference between the long and wavy lines within the fat and the straight and more uniform lines within the muscle. The Femoral Vein can be seen beneath the Femoral Artery here. Retrace with your probe to confirm structures (fall-off of the VM and appearance of the next ovoid shape) if it becomes confusing. When the local is injected, watch to see that if you crossed the Sartorius muscle, the local does not fill within the muscle itself. The local should swell the ‘collapsed triangular-shaped plane’ in which the artery and nerve reside. I don’t think it is an issue to try to determine whether or not you are within the Adductor Canal. I avoid the Sartorius more now, and I always stay out of the VM. This kind of anchoring is painful, causes more bleeding and VM contraction may significantly move the catheter tip.
Click play below to see an annotated ultrasound video displaying some of the educational points above:
Click play below to see an ultrasound video displaying characteristics of the Femoral vessels and Saphenous Nerve from a distal toward a proximal location (the Sartorius Muscle has already been located):
[/wlm_ismember]
See Also: Sartorius Muscle



